Do you have pain, cancer, or diabetes? Your PBM may now be your doctor for these illnesses.
 Charles L. Bennett MD PhD MPP, Smart State and Frank P and Jose M Fletcher Chair, Medication Safety and Efficacy, Smart State Center of Economic Excellence, University of South Carolina and the Hollings Cancer Center at the Medical University of South Carolina; Charleston, South Carolina; Email: charlesleebennett@gmail.com
Charles L. Bennett MD PhD MPP, Smart State and Frank P and Jose M Fletcher Chair, Medication Safety and Efficacy, Smart State Center of Economic Excellence, University of South Carolina and the Hollings Cancer Center at the Medical University of South Carolina; Charleston, South Carolina; Email: charlesleebennett@gmail.com
A: You and I continue to believe that medical care responsibility logically devolves to the doctor who cares for the patient and is accountable for management, treatment, and outcomes. We are increasingly wrong. Since medicines have grown in cost and pharmaceutical costs continue to increase, profit-oriented businesses muscle the patient and the doctor (and stay tuned, even the hospital) out of the way. Pharmacy Benefit Manager (PBM)’s plans now often replace physician choice, and if the physician’s choice is expensive, they replace it with more profitable alternatives, a practice known as non-medical switching. These concerns are magnified as one of the largest PBMs (CVS) seeks to merge with one of the largest health insurers (AETNA), ultimately increasing PBM involvement where patients receive care. Just as worrisome is the “invisible” hand of PBMs in restricting treatment options for chronic pain often experienced by cancer patients and others.
Can you remind us what are Pharmaceutical Benefit Managers (PBMs) and how did they get here? PBMs were developed with lofty goals to act on behalf of insurance companies and payers to maintain or reduce prescription costs while concurrently improving outcomes. These “middle men” corporations are now the principal players in our health care system, controlling at least 80% of drug benefits for 260 million Americans. The initial goal has gone astray. What started as a value-based strategy, allowing for individual case decision exceptions, morphed into blatant non-transparent and cost-based guidelines selecting from restricted lists of drugs based on the lowest cost and highest profit to the PBM, onerous prior authorization and step therapy processes, convoluted co-pays and tier formulas that disregard patient need and clinical judgment, and (in the future) requirements about where patients will receive their care.
How are PBMs handling the opioid epidemic? The impact of this ill-suited logic for pharmaceuticals is clearly demonstrated by the current opioid epidemic in the United States and the role of PBMs in driving patients to opioids, away from abuse-deterrent form (ADF) and less addictive forms of opiates through formulary and pricing strategies. “The three biggest PBMs cover no more than three FDA-approved abuse-deterrent formula opioids (Oxycontin ER, Embeda, Hysingla ER) and do not cover 7 FDA-approved abuse-deterrent formula opioids (Targinig ER, MorphaBond ER, Xtmapza ER, Troxyca ER, Arymo ER, Vantrela ER, and Roxybond). CVS Caremark, which has nearly 90 million members, doesn’t cover a single one. Only one third of Medicare prescription drug plans will cover a more pricey but less addictive opioid, and require prior authorization for other opioid alternatives. These pharmacies do, however, cover the cheaper generic opioids which are readily diverted to abusei. An Institute for Clinical Economic Review studyii found that the use of the abuse-deterrent formulation version of OcyContin could prevent 4,300 cases of abuse and save $300 million in medical costs over a five-year period. In fact, in response to PBM policies not to cover less addictive opioid alternatives led Dr. Milton Packer, the distinguished cardiologist, to conclude that payers are the leading cause of death in the United Statesiii.
How are PBMs handling oncology patient concerns? The exclusion of the patient and physician in drug choice and the emphasis on cost rather than real-world value of products is particularly worrisome for cancer patients who are on multiple medications, dealing with chronic pain, and focusing their concern over the current care rather than the risk of addiction upon survival. Data has shown that a switch to a less expensive medication for non-medical reasons leads to increased annual medical payments. Non-medical switching has been found to be associated with significantly more negative effects than benefits, even more substantial when it occurs among patients who are stable and doing well on their current treatment regimens. The social, medical, and psychological impact arising from driving patients to addictive, yet less expensive drugs, isn’t reflected in the PBM’¬¬s profits, and it isn’t included in their formulary or pricing reviews.
How are PBMs handling concerns of persons with diabetes? Diabetes is another chronic disease that has activated discussion on the problem of PBMs, rather than the physician-guiding treatment choices. The American Diabetes Association recently published a statement Aug. 15, 2017iv “ADA Deeply Concerned with Recent Prescription Drug Formulary Trends” that patient-centered approach, in consultation with a multidisciplinary diabetes care team, should be the guiding principle for making treatment choices. The action of PBMs and insurers to limit therapeutic choice through formulary exclusion or pricing “impairs a patient’s access to certain treatments and limits provider’s choice of agents that are most effective for their patients, potentially adversely affecting patient outcomes”.
What can be done? Traditionally, physician’s prescribed medicines they felt were most likely to help their patients based on clinical judgment, rather than cost alone. We recognize that lowering pharmaceutical costs in the United States is essential. However, this must be the purview of professional societies and other health care patient and provider groups, rather than that of the PBMs that profit directly for every dollar saved. In essence, the PBM has now become the physician, without, training, knowledge, medical license, knowledge of the patient (or their illness), while making medical decisions highly relevant to the patient’s care and outcomes. Stay tuned, and it will soon be your hospital as well. The solution to the problem requires a concerted effort from those most impacted, patients and providers, to encourage conversation and collaborative problem-solving. The ultimate goal is to have the physician be the doctor once again. Without these changes, public health epidemics will continue to afflict the health and well-being of our nation.
Charles Bennett’s contact info is included in the author affiliations at the top of this page.
- Pitts P, Hospital Impact – PBMs are worsening the opioid epidemic. Fierce Healthcare Aug 3., 2017. http://www.fiercehealthcare.com/hospitals/hospital-impact-pbms-are-worsening-opioid-epidemic
- Abuse Deterrent Formulations of Opioids: Effectiveness and Value. ICER June 28, 2017. https://icer-review.org/wp-content/uploads/2016/08/NECEPAC_ADF_PublicComments_062817.pdf
- Packer, M Are Payers the Leading Cause of Death in the United States? Medpage Today Sept 17, 2017. https://www.medpagetoday.com/blogs/revolutionandrevelation/68935
- American Diabetes Association American Diabetes Association Deeply Concerned with Recent Prescription Drug Formulary Trends, Press Releases Aug. 15, 2017. http://www.diabetes.org/newsroom/press-releases/2017/american-diabetes-association-deeply-concerned-with-recent-prescription-drug-formulary-trends.html?referrer=https://www.google.com/


 Gavin J. Gordon, MBA, PhD, Vice President of Commercial Operations at Fluidigm Corporation, South San Francisco, CA
Gavin J. Gordon, MBA, PhD, Vice President of Commercial Operations at Fluidigm Corporation, South San Francisco, CA
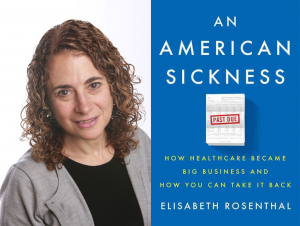 An American Sickness: How Healthcare Became Big Business and How You Can Take it Back,” the talk will look at just that. Everyone knows that the U.S. health system is by far the most expensive in the world, with spending/prices for drugs, procedures and hospitalizations that are many times those in other developed countries. And for all that, we don’t generally get better care or better results. I’ll look at the evolution of the U.S. health system over the last 3 decades and how it moved from a caring endeavor to a financially driven system where profit rather than patient good was the prime motivation. I’ll trace how commercial forces and interests were allowed to insinuate themselves into medical practice, step-by-step, so no one protested much…or even noticed…until the prices got sky high. We now live in a system where medical machinery comes with brochures on how to recoup return-on-investment and ambulance companies as well as dialysis units are owned by venture capital firms. But the ultimate message is one of optimism and hope. Once patients-voters-consumers understand how the system functions and how our healthcare has been hijacked for profit, the book offers many ways to push back, to begin untangling the mess we’re in. I discuss some of those, from strategies to protect your wallet when you enter the hospital or doctor’s office to reforms that should be voter issues at the state and national level. I believe that if patients and physicians stand up for medicine we will get better, cheaper care. The books ends: “Given the false choice between your money or your life, it’s time to take a stand for the latter.
An American Sickness: How Healthcare Became Big Business and How You Can Take it Back,” the talk will look at just that. Everyone knows that the U.S. health system is by far the most expensive in the world, with spending/prices for drugs, procedures and hospitalizations that are many times those in other developed countries. And for all that, we don’t generally get better care or better results. I’ll look at the evolution of the U.S. health system over the last 3 decades and how it moved from a caring endeavor to a financially driven system where profit rather than patient good was the prime motivation. I’ll trace how commercial forces and interests were allowed to insinuate themselves into medical practice, step-by-step, so no one protested much…or even noticed…until the prices got sky high. We now live in a system where medical machinery comes with brochures on how to recoup return-on-investment and ambulance companies as well as dialysis units are owned by venture capital firms. But the ultimate message is one of optimism and hope. Once patients-voters-consumers understand how the system functions and how our healthcare has been hijacked for profit, the book offers many ways to push back, to begin untangling the mess we’re in. I discuss some of those, from strategies to protect your wallet when you enter the hospital or doctor’s office to reforms that should be voter issues at the state and national level. I believe that if patients and physicians stand up for medicine we will get better, cheaper care. The books ends: “Given the false choice between your money or your life, it’s time to take a stand for the latter. Pramod John, PhD, CEO, VIVIO Health, San Leandro, CA;
Pramod John, PhD, CEO, VIVIO Health, San Leandro, CA; Eddy Yang, MD, PhD, Professor and Vice Chair of Translational Sciences Department of Radiation Oncology; Deputy Director, Associate Director of Precision Oncology at the Hugh Kaul Precision Medicine Institute; Birmingham, AL;
Eddy Yang, MD, PhD, Professor and Vice Chair of Translational Sciences Department of Radiation Oncology; Deputy Director, Associate Director of Precision Oncology at the Hugh Kaul Precision Medicine Institute; Birmingham, AL; Justin Stebbing, MA FRCP FRCPath PhD, Professor of Cancer Medicine and Medical Oncology at the Imperial College/Imperial Healthcare NHS Trust Charing Cross Hospital, London, UK;
Justin Stebbing, MA FRCP FRCPath PhD, Professor of Cancer Medicine and Medical Oncology at the Imperial College/Imperial Healthcare NHS Trust Charing Cross Hospital, London, UK; Lisandra West-Odell, PhD, Scientist and Product Manager, Cancer Commons, Los Altos, CA;
Lisandra West-Odell, PhD, Scientist and Product Manager, Cancer Commons, Los Altos, CA; Professor Michael Baum, Professor Emeritus of Surgery & Visiting Professor of Medical Humanities, University College, London, UK;
Professor Michael Baum, Professor Emeritus of Surgery & Visiting Professor of Medical Humanities, University College, London, UK; Diane E. Meier, MD, FACP, Director, Center to Advance Palliative Care; Professor of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai; New York, NY;
Diane E. Meier, MD, FACP, Director, Center to Advance Palliative Care; Professor of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai; New York, NY;
 Erin Maloney, Intrepid explorer, Amateur photographer, Aspiring leader; Toronto, ON;
Erin Maloney, Intrepid explorer, Amateur photographer, Aspiring leader; Toronto, ON;